Drug-Resistant Bacteria on the Rise: What Are 3 Methods of Infection Control?
A new report from the Centers for Disease Control and Prevention (CDC), is raising alarms across healthcare communities. Between 2019 and 2023, the United States saw a 460% increase in infections caused by NDM-producing carbapenem-resistant Enterobacterales (NDM-CRE) — one of the most dangerous categories of antibiotic-resistant bacteria.
These pathogens are not only resistant to most available antibiotics, but can also spread rapidly through healthcare facilities. The CDC estimates that in 2020 alone, carbapenem-resistant Enterobacterales (CRE) infections led to roughly 12,700 cases and 1,100 deaths in the U.S. The growing emergence of NDM-CRE now threatens to push those numbers even higher, reevaluating infection control efforts as priority for health workers.
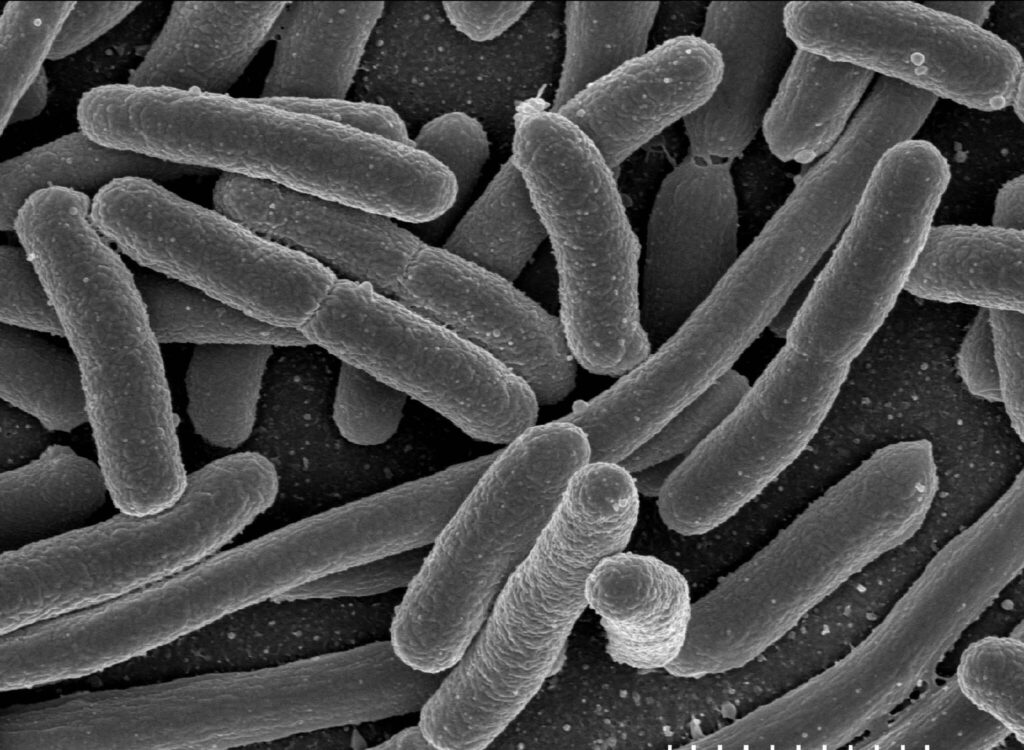
Understanding NDM-CRE
NDM-CRE belongs to a class of bacteria known as carbapenem-resistant Enterobacterales, notorious for their resistance to the most powerful antibiotics available — carbapenems. The “NDM” designation refers to New Delhi metallo-β-lactamase, which is an enzyme that enables these organisms to break down antibiotics and render them ineffective.
This resistance mechanism makes it especially dangerous, often leaving clinicians with few or no treatment options. Infections caused by NDM-CRE can lead to pneumonia, bloodstream infections, urinary tract infections, and wound infections; each are capable of severe or fatal outcomes.
While NDM-CRE was once rare in the United States, its presence has grown dramatically, prompting urgent calls for stronger surveillance and infection control measures in healthcare settings.
Why the Surge Matters
The sharp increase in NDM-CRE cases raises concerns across hospitals and long-term care facilities for several reasons:
- Difficult to treat: NDM-CRE infections are resistant to nearly all available antibiotics. Misidentifying the strain can lead to ineffective treatment and poor outcomes.
- High mortality risk: These infections carry elevated mortality rates, particularly among immunocompromised or critically ill patients.
- Rapid spread potential: Without proper infection prevention and control practices, NDM-CRE can move easily through healthcare systems and potentially into the community.
Gaps in infection prevention and limited diagnostic capacity are believed to be major contributors. Many hospitals lack access to the specialized testing needed to detect NDM-CRE promptly. Delayed identification increases transmission risk and limits treatment options.
In a conversation with Infection Control Today, Danielle Rankin, an epidemiologist in CDC’s Division of Healthcare Quality Promotion, said, “To control these organisms in healthcare settings really depends on the implementation of good infection control practices for all patients and residents in healthcare settings.” Infection preventionists (IPs) are encouraged to work closely with state and local healthcare-associated infection (HAI) programs as this is one key in preventing the spread of NDM-CRE.

3 Methods of Infection Control
Environmental cleaning plays a crucial role in disrupting bacterial spread. High-touch surfaces such as bed rails and light switches should be disinfected daily and between patient use. Shared devices like ultrasound probes must be cleaned thoroughly between each use. Sink areas also warrant special attention since bacteria can spread through splashing or surface contact. Facilities should ensure that patient supplies are not stored near sinks, and that drains are disinfected regularly. Additionally, infectious waste should be properly disposed of (e.g. not poured down a sink drain).
Healthcare organizations should renew their focus on the fundamentals of infection prevention. Ongoing education and competency checks ensure that infection control protocols are followed consistently across teams — including environmental services (EVS) and nursing staff.
The CDC provides evidence-based guidelines to help healthcare organizations navigate everyday challenges. Here are three ways your facility can prevent the spread of carbapenem-resistant Enterobacterales:
- Hand Hygiene
Frequent and proper hand hygiene remains the single most effective defense. Clinicians should clean their hands before and after every patient interaction, before performing aseptic tasks like handling indwelling medical devices, after exposure to bodily fluids, and immediately after removing gloves.
- Proper Personal Protective Equipment (PPE)
Healthcare personnel must wear gowns and gloves when caring for patients known to or suspected to be infected with CRE. Proper donning and doffing techniques help prevent self-contamination.
- Cleaning and Disinfection of Medical Equipment
Non-critical medical devices such as blood pressure cuffs and stethoscopes should be dedicated to individual patients whenever possible. If sharing is unavoidable, equipment must be disinfected after each use.
A Hidden Vector: Hospital Peripherals and Technology
Beyond patient rooms, mobile technology and shared electronics present additional risk. Medical carts, tablets, touchscreens, and phones travel between units and are frequently handled by multiple staff members throughout the day. These devices can serve as vectors for cross-contamination if not properly cleaned and disinfected.
Many computer peripherals and touchscreen devices are not designed to withstand repeated exposure to harsh disinfectants. Over time, industrial-grade cleaning agents can degrade plastics, erase keycap legends, damage screens, and shorten device lifespans — forcing costly replacements.
This is where purpose-built infection control technology becomes critical.
Durable Infection-Control Tools: Seal Shield Solutions
Seal Shield’s infection-control peripherals are designed to meet the challenges of healthcare environments. They offer products that are fully waterproof, washable, and compatible with hospital-grade disinfectants. That means, you can use harsh cleaning agents, including ones with EPA-approved claims against CRE, on our solutions without worrying about damage during routine cleaning.
Some of the popular washable keyboards and mice ideal for healthcare environments are:
- Cleanwipe Pro Keyboard: Featuring an IP68 waterproof rating and magnetic USB connector, it can be fully submerged or run through a dishwasher for deep cleaning. Its smooth surface and ergonomic design makes disinfection simple without interrupting workflows. A versatile solution perfect for medical carts, non-clinical areas, and patient rooms.
- Seal Silk Pro Keyboard: Combines mechanical typing feedback with a fully sealed silicone body for silent operation in patient areas. Its waterproof construction supports frequent cleaning, and its silicone cover acts as a noise dampener, which can help reduce noise in sensitive NICU and ICU environments.
- Seal Storm Waterproof Mice: A durable,waterproof mouse designed to handle repetitive disinfection without deterioration, ensuring reliable performance even in high-use settings.
- Clean Seal Screen Protectors: Available in standard, anti-glare, and privacy options, these protectors are built for resisting chemical damage and scratches from frequent cleaning, extending the life of screens that visit all areas of the hospital, including phones, tablets, monitors, and medical displays.
By using washable, disinfectant-ready devices, healthcare workers can maintain infection control standards without risking equipment damage — a small but significant step toward reducing bacterial transmission within hospitals.
Prevent the Spread of Drug-Resistant Bacteria
After reading the CDC’s report, you’ll see how NDM-CRE’s rise underscores how quickly gaps in testing and prevention can turn into national threats. Healthcare organizations must prioritize surveillance programs, hygiene, and access to reliable disinfection tools to maintain staff and patient safety.
To help you accomplish this, reach out to Seal Shield to learn how we support infection control efforts through washable, durable technologies built to withstand the toughest hospital cleaning protocols.


